Regulatory
- Home
- Blog
- Regulatory
- Will Digital Health Remedy or Reinforce Healthcare Inequities?
Will Digital Health Remedy or Reinforce Healthcare Inequities?

Over time, healthcare disparities in the US have widened along lines of age, race, gender, language, location, and socioeconomic status. [1] Despite rising broadband infrastructure and mobile technology over the last decade, digital adoption in rural areas has lagged behind urban communities. [2] As such, there is real concern that growth in digital health and telehealth will compound the effects of digital healthcare disparities in our most vulnerable populations. This has invoked a call to action among digital health leaders and developers to align the future of digital health design around healthcare equity for all individuals.
The Healthcare Divide meets the Digital Divide
Thirty seven percent of the US population (121 million Americans) live in “healthcare deserts.” More specifically, 80% of US counties lack adequate access to healthcare resources including pharmacies, primary care providers, hospitals, hospital beds, trauma centers and low-cost health centers. This translates to almost half of all US counties have less than 2 hospital beds per 1000 people. [3] The figure below helps conceptualizes the geographic distribution of healthcare deserts, notably which are heavily weighted in rural areas.

Image credit: https://www.goodrx.com/blog/wp-content/uploads/2021/09/GoodRx_Healthcare_Deserts_White_Paper.pdf
At first glance, leveraging technology and digital health to fill this healthcare accessibility gap may seem like a no-brainer. Which is why, when the US healthcare system was stressed by COVID-19, it quickly shifted to video-enabled tele-healthcare and online/mobile health technologies to keep it afloat. In doing so, it empowered many individuals with resources to continue to safely manage their chronic health conditions and triage acute illness. According to Medicare data, telemedicine visits made up 0.1% of all primary care visits in February, 2020 before the public health emergency; by April 2020, up to 43.5% of all primary care visits were delivered via telemedicine. [4]
Although many Americans can point to this as a lifeline during the pandemic, the 19 million Americans without broadband access were further marginalized in a digital-based health system. [5] This system took for granted that its users would require both digital access and digital literacy as prerequisites to access their provider and to longitudinally manage their care remotely. The effect of this was the widening of the healthcare divide that was already disenfranchising many vulnerable populations rather than closing it.
The digital health divide is best visualized as an overlap of regions within the US where there exist both a healthcare divide and a technology divide. Digital deserts are both rural and urban areas with limited access to internet and technology secondary to inadequate broadband infrastructure or socioeconomic limitations. It can be broken down into one or more of the following problems: lack of technology, inadequate access to broadband internet, and/or poor digital literacy. The Pew Research Center reported that 24% of rural Americans have a cell phone but not a smartphone and thus cannot use mobile health apps, patient portals, or telemedicine on the digital devices they own. Further, 1 out of every 4 elderly individuals does not use the internet and only 64% of elderly individuals have home broadband. [6] White households have higher rates of device ownership than black or Hispanic households (80.9% versus 63.9% and 67.5% respectively) and thus minority groups are more likely to depend heavily on cellular reception for internet access. [7] This divide reinforces disparities based on age, race, education, income, and location.

Image Credit: Wood BR, et al. Advancing digital health equity: a policy paper of the Infectious Disease Society of America and the HIV Medicine Association. Clin Inf Dis, 72(6):913–919.
The digital health divide is further accentuated by the challenge of digital literacy. Understanding and using digital health solutions requires both necessary cognitive and technical skills and is challenged by language/cultural barriers and physical disabilities. This is illustrated by the examples below:
(1) A patient portal requires a digital device (smart phone or computer) with baseline digital literacy to navigate to and through the portal to obtain and use the information in a timely fashion. This is now the preferred mode of communication with one’s provider.
(2) Remote patient monitoring devices with home Wifi hubs require reliable Wifi access to capture and deliver information in real-time and facilitate remote communication with the provider.
(3) A video telehealth visit requires digital literacy to efficiently use the interface, troubleshoot said interface, and a broadband connection with speeds fast enough to support streaming video.
As such, synchronous and asynchronous digital communication between a physician and the patient falls short in practicality and usability when applied to communities with poor broadband infrastructure, limited device access, and poor digital literacy.
These digital deserts are not a standalone problem; they have downstream effects on health and are directly correlated with higher-than-average rates of diabetes and obesity, both of which are considered gateway chronic medical conditions to heart disease, stroke and certain cancers. [8] The Federal Communications Commission Connect2Health Task Force has a powerful mapping tool that shows the overlay and divide between broadband access and healthcare outcomes. [9]
Without internet connectivity, during the COVID pandemic when the rates of infection were highest, a person would not be able to work from home, educate kids remotely, make an online vaccine appointment, or see their doctor through a telehealth visit. Real-world data confirms the disadvantages that these individuals faced, including:
- Video visits were under-utilized in disadvantaged communities during the COVID-19 pandemic. Audio visits were the most utilized alternative to in-person care according to data from California-based Federally Qualified Health Centers (FQHC) that service low income individuals. [10]
- A University of Pennsylvania study found profound discrepancies in telemedicine use at a large academic health center during the COVID pandemic. Unsurprisingly, older, non-English speaking females with low incomes were at risk for reduced telehealth utilization. [11]
- The digital infrastructure for online vaccine appointments created barriers for marginalized populations (older, non-white, low income) without technical resources to utilize it, contributing to the low vaccine rates of communities most affected by COVID-19. [12] In fact, in digital deserts, vaccine appointments were usurped by internet-savvy nonresidents over residents in their own communities. [13]
These examples illustrate that access to technology and connectivity are directly linked to healthcare access and patient outcomes, effectively categorizing digital access as a social determinant of health.
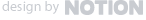
The Center for Universal Design at North Carolina State University defines Universal Design as “the design of products and environments to be usable by all people, to the greatest extent possible, without the need for adaptation or specialized design.” [14] With Universal Design, it is of utmost importance to understand the barriers specific to a community. Below, RockHealth proposes a working schematic to center health equity in product development, digital health design and deployment, and create health equity informed solutions. [15] It describes four anchors:
1) Center in the community
2) Co-design the solution
3) Develop the right tech
4) Make it accessible
Image Credit: https://rockhealth.com/insights/building-toward-equity-a-working-model-for-digital-health/
As the solution lies within its design and development, the following suggestions are guiding principles with which to design towards health equity. First, start with a diverse digital health design team. Then consider the following:
- Design systems that allow for access across varied communities
- Design at common language and literacy benchmarks
- Design technologies to avoid bias
- Develop innovative workflows with mixed forms of contact to heighten patient engagement. 90% of texts are read within 90 seconds, suggesting mobile texting as a reliable communication format.
- Develop measures to track inequities and monitor progress
- Develop education around digital literacy that is scalable
- Ensure high level cybersecurity measures are in place to protect privacy
- Engage in advocacy related to extending and expanding broadband access
- Learn from international solutions that regularly work in resource limited settings and barriers to communication. Consider how international digital solutions can be repurposed in the US.
At the speed that digital health is expanding, it is critical that these measures be taken immediately to level the field of healthcare access and to mitigate the further widening of the digital health divide. If you are reading this article, you have access to the internet, a device capable of browsing it, and the digital proficiency to access the information in a timely fashion — a circumstance that 27% (or almost 3 out of every ten) Americans are unable to achieve in 2021. [16] The need to bridge the digital health divide is admittedly daunting, however institutions and individuals stand to gain by its resolution during a time of bipartisan political will to act in urgency.
Not a moment too soon, on November 5, 2021, President Biden’s $1.2 trillion Infrastructure Investment and Jobs Act was passed in the House of Representatives, which included a historic $65 billion investment earmarked for broadband infrastructure. [17] Almost two-thirds of that investment ($42.45 billion) will be portioned for the Broadband Equity, Access, and Deployment program that would subsidize the buildout of broadband into unserved areas. The next $14.2 billion is allocated to the Affordable Connectivity Fund, which extends the pandemic’s Emergency Broadband Benefit Program, that offers a monthly $30 discount on broadband pricing for eligible low-income households. The remaining $8.35 billion is assigned to diversity, equity and inclusion efforts including grant funding for state-level programs that increase digital adoption, grants and loans to the Department of Agriculture’s Rural Utilities Service and the Tribal Broadband Connectivity Program, as well as $600 million in Private Activity Bonds. This is America’s largest investment to date in digital infrastructure in an effort to bring affordable and reliable internet access to all Americans and mitigate the digital divide.
The Roadmap Ahead: The Challenge to Narrow the Divide
With the rapid digital transformation of healthcare, there exist opportunities to address the health inequities resulting from socioeconomic status, race, gender, disabilities, location, time, and language. The goalposts for the digital transformation of healthcare have moved. The future of digital healthcare needs to create accessible, affordable healthcare delivered through an enhanced patient experience with easy usability that improves outcomes for all individuals while adding value to the population.
This mission will require a multipronged approach at the level of the individual, the community, and the digital health system overall. The most vulnerable populations living in healthcare and digital deserts stand to benefit the most through reliable access to and usability of digital health and its delivery. Although ambitious, to fail at this challenge will further disenfranchise vulnerable individuals and communities in an irreversible way with little recourse in the future. It is imperative that we closely study and purposefully create a healthcare system that prioritizes equitable access to digital health solutions.
References
- Gibbons, MC. A historical overview of health disparities and the potential of eHealth solutions. JMIR 2005;7(5):e50.
- https://www.pewresearch.org/fact-tank/2021/08/19/some-digital-divides-persist-between-rural-urban-and-suburban-america/
- https://www.goodrx.com/blog/wp-content/uploads/2021/09/GoodRx_Healthcare_Deserts_White_Paper.pdf
- https://aspe.hhs.gov/reports/medicare-beneficiary-use-telehealth-visits-early-data-start-covid-19-pandemic
- https://www.fcc.gov/reports-research/reports/broadband-progress-reports/eighth-broadband-progress-report
- https://www.pewresearch.org/internet/fact-sheet/internet-broadband/
- Wood BR, et al. Advancing digital health equity: a policy paper of the Infectious Disease Society of America and the HIV Medicine Association. Clin Inf Dis, 72(6):913–919.
- https://www.fcc.gov/health/maps
- https://www.fcc.gov/reports-research/maps/connect2health/background.html
- Uscher-Pines L , et al. Telehealth use among safety-net organizations in California during the COVID-19 pandemic. JAMA. 2021;325(11):1106–1107.
- Eberly et al. Telemedicine outpatient cardiovascular care during the COVID-19 pandemic: bridging or opening he digital divide? Circulation 2020:142:510–2.
- https://www.kff.org/policy-watch/early-state-vaccination-data-raise-warning-flags-racial-equity/
- https://www.propublica.org/article/memphis-area-residents-without-internet-must-wait-days-for-vaccination-appointments-while-others-go-to-the-front-of-the-line
- Story MF . Maximizing usability: the principles of universal design. Assist Technol. 1998;10(1):4–12.
- https://rockhealth.com/insights/building-toward-equity-a-working-model-for-digital-health/
- https://www.pewtrusts.org/en/trust/archive/summer-2019/americas-digital-divide
- https://arstechnica.com/tech-policy/2021/11/congress-oks-42-billion-to-deploy-100mbps-broadband-in-unserved-areas/
A registered 501c3 non-profit organization, we help healthcare organizations realize the benefits of digital medicine faster and with less risk by creating, gathering, and sharing clinical evidence and best practice
Copyright © 2026 NODE.Health. All Rights Reserved.